
Niger J Paed 2016; 43 (1): 58 – 61
CASE
REPORT
Oyinlade OA
Subacute combined degeneration of
Lagunju IA
Balogun TAB
the spinal cord in a Nigerian child: a
Famosaya AA
need for a high index of suspicion
DOI:http://dx.doi.org/10.4314/njp.v43i1.12
Accepted: 19th December 2015
Abstract :
Background: Vitamin
from follow up for 8 years after
B12 deficiency has been reported
which
he
represented
with
Oyinlade OA (
)
to
be associated with a spectrum
paraparesis and urinary inconti-
Lagunju IA
of
neurological disorders among
nence. He was managed again with
Department of Paediatrics,
College of Medicine, University of
which is subacute combined de-
parentheral vitamin B12 prepara-
Ibadan / University College Hospital,
generation of the spinal cord.
tions with good outcome and total
Ibadan, Nigeria.
Method: We
report a
case of
resolution of symptoms at dis-
Email: ladealex2005@yahoo.com
subacute combined degeneration
charge.
of
the spinal cord secondary to
Conclusion :
A high
index of
suspi-
Balogun TAB, Famosaya AA
vitamin B12 deficiency and dis-
cion is needed in identifying vita-
Department of Paediatrics,
cussed the clinical presentation
min
B12
deficiency
related
University College Hospital, Ibadan
and management challenge.
paraparesis in paediatric practice
Nigeria.
Result :
The diagnosis
was made
while the need for indefinite treat-
through a high index of suspicion
ment
and follow up is hereby em-
when
the clinical presentation
phasized.
ranked highly with the mode of
presentation of Vitamin B12 defi-
Key words:
Vitamin
B12
defi-
ciency. Patient responded well to
ciency; myelinopathy; parapare-
parentheral vitamin B12 prepara-
sis; subacute combined degenera-
tion but subsequently defaulted
Introduction
Subacute Combined Degeneration of the Spinal Cord
Vitamin B12 (Cobalamin) deficiency results in a wide
(SCDSC), a condition which could result from vitamin
range of haematological and gastrointestinal disorders. It
B12 deficiency can present with varying degree of im-
is
well known to be associated with myelinopathy, pe-
pairment of spinal cord functions, often heralded by
ripheral neuropathy, optic neuropathy, memory loss,
posterior column dysfunctions which could manifest as
neuropsychiatry disorders and subacute combined de-
impairment of joint position and vibration sense, ataxia
generation of the spinal cord
(1-4)
.
It is a condition that is
and paraesthesia all of which could be accompanied by
relatively commoner in adult than in the paediatric age
varying degree of paresis, increased deep tendon re-
group .
5
flexes, urinary incontinence and urinary tract infections
2,3,5,9,12
.
The most frequent causes of Cobalamin deficiency are
malabsorption which may follow pernicious anaemia,
In
the nervous system, Vitamin B12 acts as a co-enzyme
gastrectomy, intestinal infections, tropical sprue and
in
the methyl-malonyl-CoA mutase pathway necessary
pancreatic exocrine insufficiency . Inadequate absorp-
1,5
for myelin synthesis. Hence, its deficiency results in
tion can also result from deficiency of intrinsic factor, a
defective myelin synthesis resulting in central and pe-
ripheral nervous system dysfunction . Normal plasma
4
glycoprotein responsible for enhancing the absorption of
Vitamin B12 from the terminal ileum and hereditary
6
concentration of vitamin B12 does not exclude the diag-
nosis of vitamin B12 deficiency . Hence, there is need
13
partial transcobalamin II deficiency . Inadequate intake
7
of
vitamin B12 has also been implicated as a major
for a high index of suspicion in diagnosing Vitamin B12
cause of its deficiency especially in vegetarians, simply
associated SCDSC, especially in paediatric age group
because vitamin B12 is mainly sourced from animal
where it is relatively rarer compared to the adult popula-
products
1,5, 8-10
.
Other recognized causes include side
tion.
effect of Nitric Oxide, an inhalational general anaes-
thetic agent, usage of which can precipitate Vitamin B12
The most consistent Magnetic Resonance Imaging
deficiency post operatively with its attendant sequelae or
(MRI) finding in SCDSC is a symmetrical abnormally
when
employed in substance abuse by adolescents
2,5,11
.
increased T2 signal intensity confined to the posterior or
59
posterio-lateral column
4,14
while some pathological find-
tion senses were difficult to assess. Liver was palpable
ings could be multifocal and vacuolated lesions . Early
9
4cm below the right costal margin, smooth and non-
diagnosis and treatment of Subacute Combined Degen-
tender. Other systemic findings were within normal
eration of the Spinal Cord is important in reversibility of
limit.
neuro-deficits and prevention of permanent neurological
damage . Promptly diagnosed patients respond dramati-
9
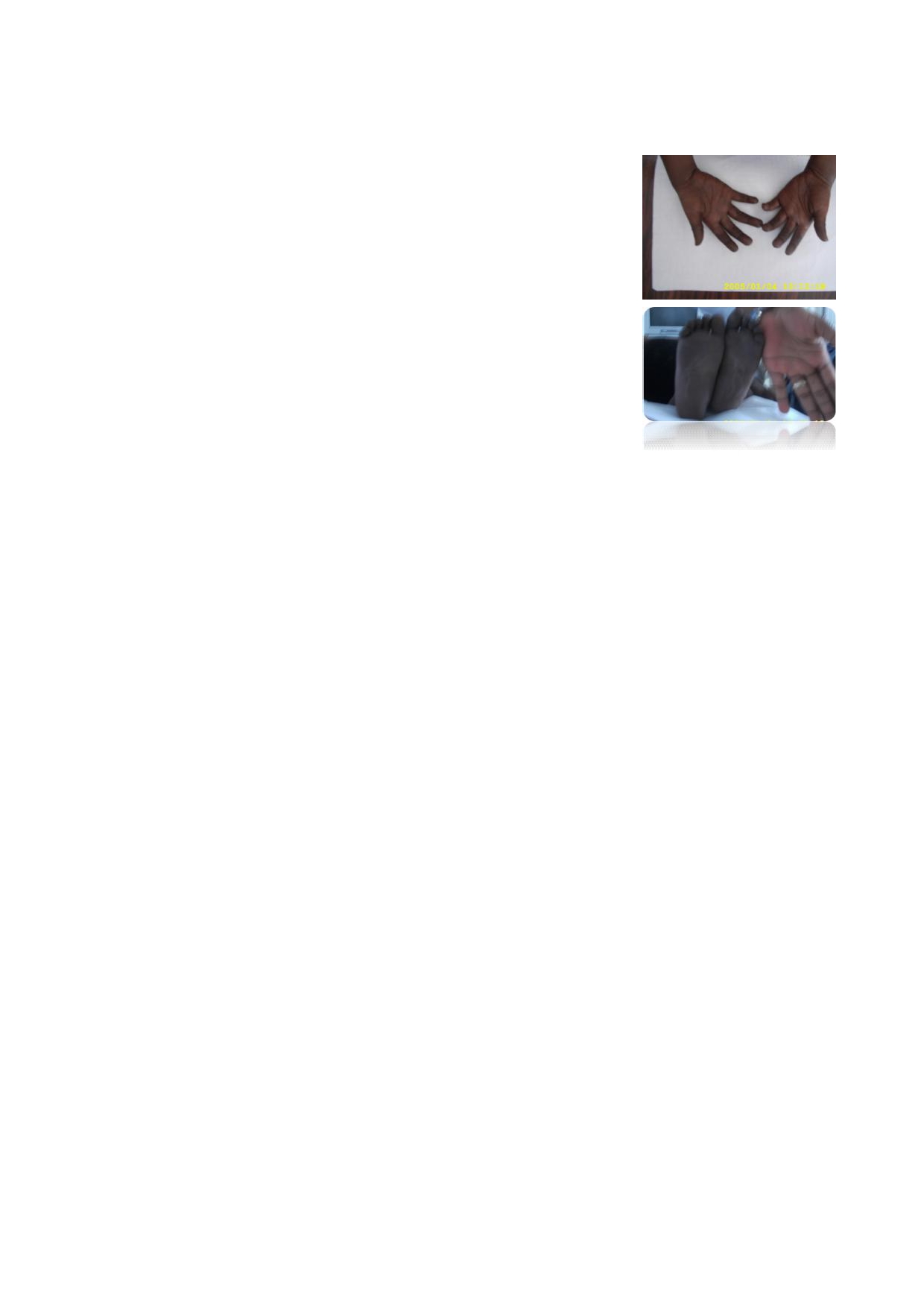
Fig 1: Hyperpigmented
cally to parentheral Vitamin B12 preparations with im-
palms
provement in neurological functions and prevention of
irreversible neuro disabilities.
We
report this case to sensitize physicians to a high in-
dex of suspicion of this condition while managing chil-
dren presenting with paraparesis.
Fig 2: Hyperpigmented
Case report
soles. The examiner’s hand
was
included for compari-
son
A
4-year-old boy presented at the Paediatric Neurology
Clinic of University College Hospital (UCH), Ibadan on
account of poor growth and recurrent fever of three
years duration, darkening of the palms and feet of 2
years duration, difficulty with walking of 3 weeks dura-
tion
and 2 days history of passage of loose stool.
An
assessment of possible Vitamin B12 deficiency with
Patient’s illness dated back to 3 years before presenta-
chronic
anaemia, spastic paraparesis, recurrent glossitis
tion
when mother noticed poor weight gain despite good
and
recurrent bacterial infections was made. Full Blood
appetite. He had associated recurrent episodes of fever
Count with Mean Cell Volume (MCV), Mean Corposcu-
and
had been treated on outpatient basis for recurrent
lar Haemoglobin Concentration (MCHC) and Mean
acute respirarory tract infections, otitis media and diar-
Corposcular Haemoglobin were requested all of which
rhoea. About 2 years prior to presentation, he was ob-
were elevated except MCHC. [MCH= 34.7pg (Ref
served to have developed progressive darkening of the
range: 26.5-33.5pg); MCHC = 32.8g/dl (Ref range: 31.5
palms and soles. There was no associated hyper pigmen-
-35.5g/dl); MCV=106 fl (Ref range: 80-97fl)]. Red cell
tation in any other part of the body. He was pale most of
morphology revealed macrocytosis and hypochromasia.
the time with associated effort intolerance and inability
He
was forthwith commenced on intramuscular (IM)
to
play as his peers. His Packed Cell Volume (PCV)
Vitamin B12 1mg alternate days for 2 weeks, then 1mg
ranged from 17%-25% from then till presentation at the
weekly for 6 weeks, then 1mg monthly. Two weeks into
neurology clinic. Haemoglobin genotype was AS.
the therapy, he made a remarkable clinical improvement
There were associated recurrent episodes of mouth ul-
evident by his ability to walk better and improvement in
cers with redness of the tongue, easy bruising and diffi-
appetite. PCV then was 35%. He was thereafter sched-
culty with eating in the 10 months preceding presenta-
uled for another follow-up in 6 weeks. However, patient
tion; and at about 3 weeks prior to presentation, he de-
defaulted from clinical care because mother felt it was
veloped difficulty with walking. Tremors of the hands
no
longer necessary and was lost to follow-up.
were also observed while the patient fed himself. There
was no history of seizures.
He
represented 8 years later on account of difficulty
with walking of 3 weeks duration, passage of bloody
He
started schooling at age 2 1/2 years but has been ir-
urine of 1 week duration and urinary incontinence of 3
regular in school due to recurrent illnesses. Pregnancy,
days duration. Persistence of hyperpigmentation of the
labour and delivery history were not contributory and
palms and soles earlier noted were observed on evalua-
developmental milestones were essentially within nor-
tion. He was unable to walk unaided with grade 4 mus-
mal limits. He was born into a polygamous setting and
cle power in both lower limbs and normal muscle power
there was no history of similar illness in the family.
in
both upper limbs. Muscle tone and deep tendon re-
Findings on examination revealed a male child with
flexes were increased in both lower limbs with impair-
sparse depigmented hair. He was a febrile, anicteric with
ment of joint position and vibration sense and bilateral
satisfactory hydration status. He weighed 13.5 kg (96%
extensor plantar responses. A diagnosis of Vitamin B12
of
expected) and had hyper pigmentation of the palms
deficiency with SCDSC, spastic paraparesis, impaired
and soles (figures 1 and 2). Grade II digital clubbing
joint position and vibration sense and urinary inconti-
were noted. He was conscious and alert with normal
nence with Urinary Tract Infection (UTI) were made.
speech, occipitofrontal circumference was 50cm which
was normal for his age. There was no cranial nerve defi-
He
was readmitted and commenced on IM Vitamin B12
cit. He had ataxic gait and was unable to tandem walk.
1mg alternate days for 2 weeks, then 1 mg weekly for 6
The muscle power was grade 4 in all limbs. The muscle
weeks. Urine Microscopy Culture and Sensitivity
tone was increased in the lower limbs whilst the deep
yielded E. coli for which he had oral cefixime for 1
tendon reflexes were exaggerated in all limbs. There was
week while Spinal Magnetic Resonance Imaging (MRI)
no
sustained ankle clonus and joint position and vibra-
showed essentially normal findings. He was also com-

60
menced on physiotherapy. MCV, MCHC and MCH val-
Vitamin B12 deficiency in this patient could not be as-
ues were increased with presence of macrocytes in the
certained due to paucity of facilities for diagnosis, a pos-
peripheral blood film [MCH=35.4 pg (Ref range: 26.5-
sible postulate is that this might have resulted from
33.5pg); MCHC=39.8 g/dl. (Ref range:31.5-35.5g/dl);
malabsorption probably secondary to lack of intrinsic
MCV= 98.7 fl (Ref range: 80-97fl)] Serum Vitamin B12
factor as history did not suggest inadequate dietary in-
and
Folic acid assays were requested but results were
take, previous gastric surgery or inflammatory bowel
still pending as at the last clinic visit. After 2 weeks of
disease. The absence of similar illness in the family also
his
management, he regained both day and night conti-
makes the possibility of hereditary transcobalamin II
deficiency unlikely . The skewing of haematological
7
nence and could walk unaided. He was discharged home
after 3 weeks on admission and prior to discharge, the
parameters (MCV, MCHC, MCH) beyond the upper
patient and his caregivers were counseled on the need to
limit of normal and the presence of macrocytes in the
complete the subsequent doses of Vitamin B12 injection
peripheral blood film during the second admission of
on
outpatient basis and continue IM Vitamin B12 1mg
this patient indicate an evolution of megaloblastic anae-
at
least 2 monthly indefinitely. The possibility of irre-
mia which is a characteristic haematological manifesta-
tion of vitamin B12 deficiency .
9
versible neurological damage which could result from
non-compliance was also extensively discussed with
them before discharge. Clinical improvement was sus-
It
is pertinent to note that SCDSC could persist despite
tained when he was last reviewed 12 days after dis-
Vitamin B12 administration in some patients with clini-
charge. He was subsequently scheduled for another fol-
cal and radiological features of SCDSC similar to that
secondary to Vitamin B12 deficiency
.(15)
low-up visit in 4 weeks.
When
this oc-
curs, the possibility of other metabolic problems such as
hypocupricemia (Copper deficiency) should be sought.
Hypocupric (Copper deficiency) myelopathy is a myelo-
Discussion
pathy which is clinically and radiologically indistin-
guishable from SCDSC due to Vitamin B12 defi-
ciency .
15
This report illustrates a classical clinical presentation of
SCDSC secondary to Vitamin B12 deficiency. The his-
tory of difficulty with walking and the physical exami-
nation findings of ataxia, paraparesis, increased deep
tendon reflexes and impairment of joint position and
Conclusions
vibration sense together with the dramatic response to
parentheral Vitamin B12 supplements all agree with this
This patient presented with classical clinical picture in
assertion as previously reported in the literatures
2,3,8
.
keeping with SCDSC secondary to Vitamin B12 defi-
The younger age and normal anatomical findings on
ciency. There is need to keep a possibility of Vitamin
spinal neuroimaging in this patient likely contributed to
B12 deficiency in view while evaluating and managing
the favourable outcome of his management, more-so
patients with paraparesis, especially when such patients
that
previous reports have shown strong correlation
fail
to respond to conventional management of common
between presence of anatomical lesions on spinal neuro
aetiologies of paraparesis in paediatric age group. The
imaging of patients with Vitamin B12 deficiency-related
recurrence of this condition in this patient further illus-
SCDSC and permanent neurological damage .
4,9
trates the consequence of neglecting a cheap and highly
effective therapy and the need for an indefinite follow-
Although the exact aetiological agent responsible for
up
and treatment.
References
1.
Gursoy AE, Kolukisa M, Babacan-
3.
Vasconcelos OM, Poehm EH,
6.
Arthur G, Hall J. Textbook of
Yuldiz G, Celebi A. Subacute
McCarter RJ, Campbel WW, Qu-
Medical Physiology. In: Belfus L,
Combined Degeneration of the
ezado ZMN. Potential outcome
Schmitt W, editors. 11th ed. Phila-
Spinal Cord due to Different Eti-
factors in subacute combined de-
delphia: Elsevier Saunders; 2006:
ologies and Improvement of MRI
generation: Review of observation
e820.
Findings. Case Rep Neurol Med
studies. J
Gen Intern
Med.
7.
Teplitsky V, Huminer D, Zoldan J,
[Internet]. 2013: 159649. Avail-
2006;1063-1068 .
Pitlik S, Shohat M. Hereditary
able from:http://www. pubmed-
4.
Briani C, Torre CD, Citton V,
partial transcobalamin II defi-
central.nih.gov/articlerender.fcgi?
Manara R, Pompanin S, Binotto G,
ciency with neurologic mental and
artid=3623262&tool=pmcentrez
et
al. Cobalamin deficiency: Clini-
haematologic abnormalities in
&rendertype=abstract Accessed on
cal
picture and radiological find-
children and adults. Isr
Med Assoc
14
May, 2015.
th
ings. Nutrients.
2013; 5
(11): 4521
J. 2003; 5(12): 868-72.
2.
Ungey C. Effect of Vitamin B12
-39.
8.
Tukuhashi H, Ito S, Hidrano S,
in
pernicious anaemia and
5.
Cabrerizo-Garcia JL, Sebastian-
Muri M, Suganuma Y, Hatturi T.
subacute combined degeneration
Royo M, Montes N, Zalba-Etayo
Subacute combined degeneration
of
the cord. Br
Med J.
1951;152 –
B.
Subacute Combined spinal Cord
of
the spinal cord in vegetarians:
7.
degeneration and pancytopaenia
Vegetarians myelopathy. Clin Pae-
secondary to severe vitamin B12 defi-
diatr (Phila). 2006; 705-6.
ciency. Sao
Paulo Med
J. 2012;
130
(4) 259-62.

61
9.
Miscusi M, Testaverde L, Rago A,
12.
Srikanth SG, Jayakumar PN,
14.
Jain KK, Malhotra HS, Garg RK,
Raco A, Colonnese C. Subacute
Vasudev MK, Taly AB,
Gupta PK, Roy B, Gupta RK.
combined degeneration without
Chandrashekar HS. MRI in
Prevalence of MR imaging abnor-
nutritional anaemia. J Clin Neuro-
subacute combined degeneration
malities in vitamin B12 deficiency
sci
[Internet]. Elsevier Ltd; 2012;
of
spinal cord: a case report and
patients presenting with clinical
19(12): 1744-5. Available from:
review of literature. Neurology
features of subacute combined
http://dx.doi.org/10.1016/
India. 2002. 310-2.
degeneration of the spinal cord. J
jocn.2012.01.039 Accessed on 16
th
13.
Gowdappa HB, Mahesh M,
Neurol Sci [Internet]. Elsevier BV;
May, 2015.
Murthy KV, Narahari MG. Helico-
2014; 342 (1-2): 162-6. Available
10.
De Rosa A, Rossi F, Lieto M,
bacter pylori associated vitamin B
from: http://dx.doi.org/10.1016/
Bruno R, De Renzo A, Palma V et
12
deficiency, pernicious anaemia
j.jocn.2011.08.028 Accessed on
16
May, 2015.
th
al.
Subacute combined degenera-
and
subacute combined degenera-
tion of the spinal cord in a vegan.
tion of the spinal cord. BMJ Case
15.
Tsang BKT, Crump N, MacDonell
Clin Neurol Neurosurg. 2012; 114
Rep. 2013; 2013(sep29_1): 10-3.
RA.
Subacute combined degenera-
(7): 1000-2.
tion of the spinal cord despite pro-
11.
Walsh LE, Garg BP. Poisoning
phylactic vitamin b12 treatment. J
and
Drug-Induced Neurologic
Clin Neurosci [Internet]. Elsevier
diseases. In: Kryhl L, Gallard J
Ltd; 2012; 19(6): 908-10.
eds. Paediatric Neurology: Princi-
Available from: http://dx.doi.org/
ple
and practice. 5 ed. Canada:
th
10.1016/jocn.2011.08.028 Ac-
cessed on 16 May, 2015.
th
Elsevier; 2012. e1745.